(Make sure you check the new update at the end concerning the recenly published study about tanning beds and melanoma!)
So what if I told you that the sunscreen you slather on yourself whenever you go out in the sun may have led to an epidemic of the deadliest form of skin cancer known-melanoma! Would you be shocked in disbelief? You should be as you have been lied to for many years about how dangerous the sun is. While hard core sun tanning can lead to a 150% to 200% increase in the risk of the least dangerous skin cancers, basal cell, and squamous cell, the increase in the risk of the deadly form of cancer, melanoma, is only about 50%. 50% sounds like a lot, but melanoma is actually the rarest form of the common skin cancers-but it is the deadliest. it is the one you really want to avoid. While extreme tanning can increase the risk of melanoma, sun avoidance and sunscreen use can increase the risk of melaonoma even more!! How can this be? You will soon see.
Basal cell and squamous cell cancers make up about 90% of all skin cancers, with basal cell comprising about 70%, and squamous cell about 20%. The deadliest skin cancer , melanoma, makes up only 10% of skin cancers but results in 90% of skin cancer deaths. The highest rates of melanoma occur in Australian and New Zealanders who get melanoma at a rate about 3X higher than North Amercians.
Alright, yes , sunscreen does protect against two “better” forms of skin cancer, basal cell carcinoma, and squamous cell , which if you had to get cancer would be the ones you would choose. Why?
Basal cell carcinoma often is more of a nuisance than a health issue if it stops growing. It almost never spreads, catch it early and there is almost no chance that it will harm you. and you can just cut it or burn it off and forget about it.
What is a basal cell? Basal cells produce new skin cells as old ones die. Limiting sun exposure can help prevent these cells from becoming cancerous. This cancer typically appears as a white waxy lump or a brown scaly patch on sun-exposed areas, such as the face and neck. Treatments include prescription creams or surgery to remove the cancer. Basal cell carcinoma is a type of skin cancer that begins in the basal cells. It’s the least risky type of skin cancer. As long as you catch it early, you can be cured.


Squamous cell cancer-Squamous-cell skin cancer (SCC) is commonly a red, scaling, thickened patch on sun-exposed skin. Some are firm hard nodules and dome shaped like keratoacanthomas. Ulceration and bleeding may occur. When SCC is not treated, it may develop into a large mass. Squamous-cell is the second most common skin cancer. It is dangerous, but not nearly as dangerous as a melanoma.


So what about melanoma? How does sunscreen cause it? I will present some evidence that shows that the epidemic of deadly melanoma that has been exploding since the 1980’s is caused by widespread sunscreen use which leads to Vitamin D3 deficiency. Being Vitamin D3 deficient makes one more susceptible to every type of cancer there is-including the deadly melanoma.

From Wikipedia: https://en.wikipedia.org/wiki/Melanoma
Melanoma, also known as malignant melanoma, is a type of cancer that develops from the pigment-containing cells known as melanocytes. Melanomas typically occur in the skin, but may rarely occur in the mouth, intestines, or eye. Melanoma often starts off as a mole.
Melanoma (the deadliest form of skin cancer) most often occurs in Asians, Filipinos, Indonesians, and native Hawaiians in places you’d least expect it, like the palms, soles of feet, and underneath the nails, says Bowe. Be sure to check these areas and to look at nails without polish to see if there are any stripes growing underneath your nail bed.

Consder the following chart:
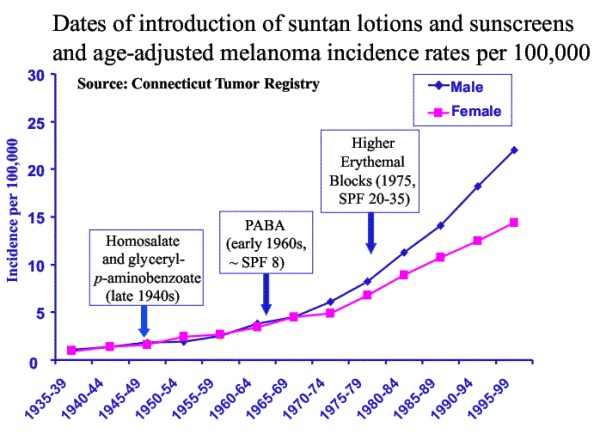
Somehow it seems the use of sunscreen is actually causing an explosion of melanoma!
I think a picture is worth 1,000 words, how about this one>>
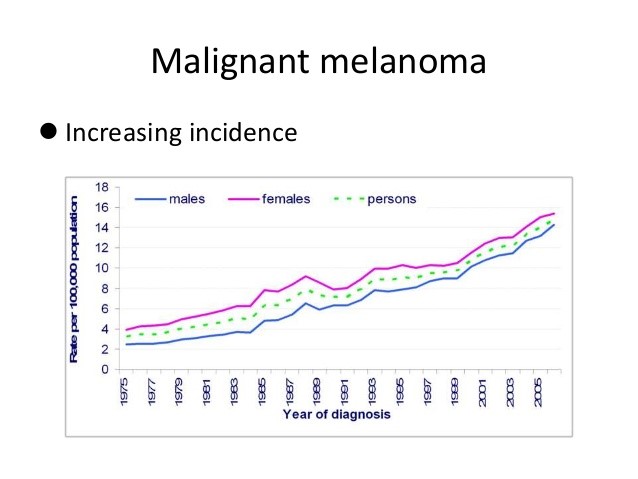
So sunscreen protects against cancer by preventing UV damage to the skin, but it also INCREASES the risk of all cancers including skin cancer by leading to a reduction in Vitamin D3 levels! Based on the charts above showing the huge rise in cases of melanoma since the widespread adoption of sunscreen use and sun avoidance, it can be logically inferred that sunscreen is doing way more harm than good!
Consider this study’s conclusions>>
PLoS One. 2014 Dec 1;9(12):e112863. doi: 10.1371/journal.pone.0112863. eCollection 2014.
Low serum 25-hydroxyvitamin d concentrations are associated with increased risk for melanoma and unfavourable prognosis.
BACKGROUND:
Low vitamin D status (serum 25(OH)D concentration) is associated with increased incidence and unfavourable outcome of various types of cancer. However, there are limited data on influence of serum 25(OH)D on risk and prognosis of malignant melanoma.
METHODS:
Basal serum 25(OH)D concentrations were retrospectively analyzed in a cohort of melanoma patients (n = 324) and healthy controls (n = 141). We tested the hypothesis that serum 25(OH)D concentrations are predictive of melanoma risk, thickness of primary melanomas, and overall survival (OS).
RESULTS:
Median serum 25(OH)D concentrations were significantly lower (p = 0.004) in melanoma patients (median = 13.6 ng/ml) as compared to controls (median = 15.6 ng/ml). Primary tumors of patients with low serum 25(OH)D concentrations (<10 ng/ml) had significantly (p = 0.006) greater Breslow thickness (median: 1.9 mm) as compared to patients with higher levels (>20 ng/ml; median: 1.00 mm). Patients with 25(OH)D serum concentrations in the lowest quartile had inferior overall survival (median: 80 months) comparing with the highest quartile (median: 195 months; p = 0.049).
CONCLUSIONS:
Our data support the concept that serum 25(OH)D concentrations are associated with risk and prognosis of melanoma. Whether normalizing serum 25(OH)D concentrations in these patients improves outcomes will require testing in future clinical trials.
So the bottom line conclusion that can be drawn is that if your only choice is to use sunscreen or not, you are more likley to die from skin cancer (as well as any other cancer) from using sunscreen and you would be smart to avoid it. You make your Vitamin D3 naturally when sunlight hits your unprotected skin.
By using sunscreen you are reducing the risk of getting the relatively easily survivable skin cancers. However this is a HORRIBLE trade off. By reducing your Vitamin D3 levels you are dramatically increasing your risk of getting all other cancers, as well as evey autoimmune disease known to man including MS, skin diseases, allegies, asthma, etc. if you doubt this is true please see this very important article on this blog site>>
OVERWHELMING PROOF THAT VITAMIN D3 DEFICIENCY CAUSES MOST HUMAN DISEASES
There is a third option, however, simply take a daily Vitamin D3 supplement of at least 5,000 IU per day and then you can still safely use sunscreen if you expect to be in overly intense sun.
Here is the new study that just came out concerning taning beds and melanoma risk- responsible tanning as required by professional tanning bed salon operators basically does not increase melanoma risk! Home tanning , which is much more likely to lead to bad sunburns does. Here it is>>
Commercial tanning salons and melanoma risk
Abstract
There have been many case-control studies of melanoma and the use of indoor tanning equipment. A recent meta analysis of 8 credible studies in North America estimated an overall significant odds ratio of 1.23. Three of these 8 studies also reported separately on commercial use and home use of indoor tanning equipment. For home use the overall odds ratio was a significant 1.53 while for commercial use there was a non significant 1.05.
Sir, In 2006, a working group of the International Agency for Research on Cancer (IARC) published a systematic review and meta analysis of epidemiological and experimental studies on the use of indoor tanning equipment and skin cancer.1 Indoor tanning equipment, as defined in the 2006 IARC report, included sunbeds and sunlamps, whether used in commercial tanning salons or other settings, and was referred to in the report as “sunbeds or indoor tanning equipment.” The authors did not separate data by place of use. Based on 19 informative studies, ever-use of sunbeds was positively associated with melanoma (summary relative risk, 1.15; 95% CI, 1.00–1.31).
In 2012, the 2006 IARC report was updated by 4 of its authors to include an additional 8 indoor tanning studies published since the IARC report.2 The term “sunbeds” was again used to refer to use of indoor tanning equipment, whether in commercial tanning salons or at home or in other settings. Based on these 27 studies of ever having used sunbeds, there was an associated summary relative risk of 1.20; (95% CI, 1.08–1.34). As in the 2006 IARC report, the authors did not separate data by place of use.
In 2014, a further systematic review and meta analysis on melanoma risk and “indoor tanning” was published.3 This study also combined data from home use with data from commercial tanning salon use, using the omnibus term “indoor tanning” to describe both. This study is the only meta-analysis on the subject that separated studies by geographical area. Figure 2 in their paper gives the odds ratios of melanoma for ever use versus never use of indoor tanning. For North America, the authors considered 8 studies to be credible and they calculated a meta analysis giving an overall odds ratio of melanoma of 1.23 (95% C.I. 1.03, 1.47) for ever having used indoor tanning; a statistically significant increase. As indicated, these individual studies combined data from indoor tanning at home and indoor tanning at commercial tanning salons. 3 of these 8 acceptable North American studies4-7 also provided a separate analysis of home and commercial tanning salon use. These analyses, as well as a meta analysis and the original analysis of the 8 studies3 are given in Table 1.
The 3 studies that considered both home and commercial indoor tanning show a considerable difference in melanoma risk between home indoor tanning and commercial tanning salon indoor tanning. The tanning salon meta analysis estimate of 1.05 essentially shows no increase melanoma effect, while the home tanning estimates a significant increase in melanoma risk. We therefore see that there is an important underlying difference between commercial tanning and “do it yourself” home tanning, which may involve increased sun burns and their known risk for melanoma.
In 2011, a report8 was presented at the 3rd North American Congress of Epidemiology held in Montreal which analyzed home vs. salon use of indoor tanning based on those studies in the original IARC report of 2006. The authors also concluded in their abstract that “When professional sunbed usage is considered independent of home and medical exposures there is no association with melanoma.”
Finally, it should be said that all of the above odds ratio values may be high due to the general problem of recall bias. (END recent study update,)
I recently updated this article to add what you have just read. What follows is the article as it originally appeared.
You always hear people say to put on sunscreen when outside to prevent skin cancer. While the use of sunscreen helps protect the skin, it can also result to your body not getting enough vitamin D.
The Journal of the American Osteopathic Association published a clinical review, which revealed that nearly one billion people worldwide are likely deficient in vitamin D due to lack of exposure to sunlight related to sunscreen use.
An increasing number of people prefer to stay indoors. When they are outside, they wear sunscreen as protection against skin cancer. Sunscreen use lessens the body’s ability to produce vitamin D from sun exposure, according to Touro University assistant professor and study researcher, Kim Pfotenhauer, DO.

Vitamin D
Vitamin D is a hormone produced by the body through sunlight exposure. It is essential for the body in absorbing calcium and phosphorous. This hormone also plays a vital role in various body functions. According to the US National Library of Medicine, a deficiency in vitamin D can cause health problems including loss of bone density. It might also contribute to health issues such as cancer, high blood pressure, diabetes, and several autoimmune disorders. Symptoms of vitamin D deficiency include bone fractures and muscle weakness.
How to Maintain Vitamin D Levels?
To get enough vitamin D, you need to spend about five minutes to half an hour under the sun during midday. Do this twice a week without using sunscreen. You can go sunbathing or do some walking under the sun to get enough sunlight. Sunscreen with SPF 15 and higher decreases the production of vitamin D3 by 99%.

There are also vitamin D supplements you can take to maintain your vitamin D levels. You can also get vitamin D from several food sources such as cereals, yogurt, milk, orange juice, and some mushrooms. There are also some fish that are good sources of vitamin D such as swordfish, tuna, sardines, and salmon.
Please note that in order to generate D3 one needs to expose more than 40% skin to UVB radiation, which has the maximum +-1h from the local zenith. Outside of that window the UVB amount is insignificant for D3 generation on the skin.
The fact that UVB is the promotor of generation of this prehormone it is important to observe the max UVB window.
I live in the 10N latitude and I usually take 15-30 minimum twice a week at noon.
kind regards,
Arsca, M.Sc. Met