LUPUS IS EASILY CURED WITH LONGER TERM
HIGH DOSE VITAMIN D3 THERAPY- CASE STUDIES- #15
The clues are all there- Lupus is obviously a Vitamin D3 deficiency disease and thus can be cured with longer-term high-dose Vitamin D3 therapy, (just like all other autoimmune diseases are proving to be cureable with D3.)
The clues-
-It affects women at a much higher rate than men (90% vs 10%).
-It affects darker-pigmented people (who tend to make less Vitamin D3 from the sun) at a much higher rate than caucasians (2.5X higher rate)
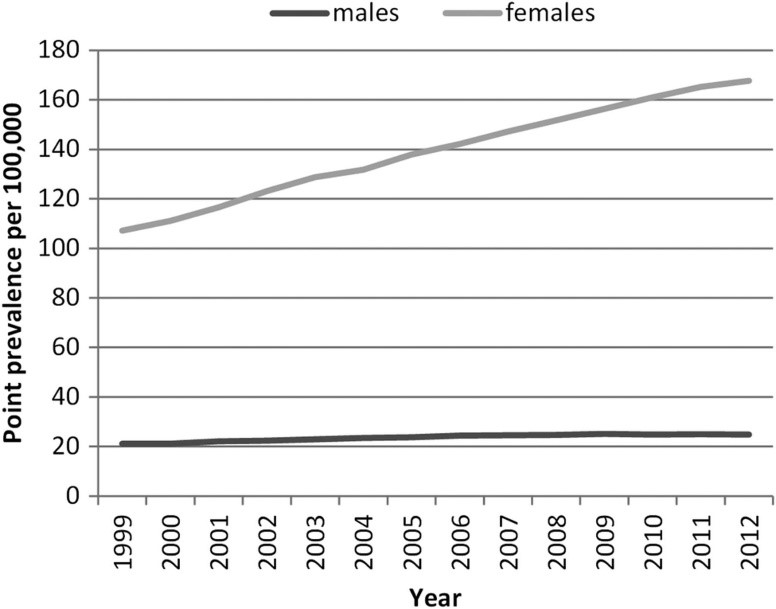
-The incidence of lupus has been increasing since 1980 when sun screen use and sun avoidance began increasing in popularity (see chart at end of article)
-There seems to be a latitude effect where the further from the equator, the weaker the sun, and thus the lower the population’s overall Vitamin D3 levels.
(Note to researchers-The research here is sketchy-the world needs a comprehensive study of lupus vs. latitude please.)
Keep in mind that Vitamin D3 is not a vitamin at all but rather a powerful immune/tissue modulating/remodeling hormone that controls at least 300 and possibly up to 2,000 of your genes-many of which are involved with your immune system.
There also exists a hierarchy of gene activation / suppression where quite a few genes are only affected at higher levels of Vitamin D3 and this has only been tested at blood levels of Ivtamin D3 at 40 ng/ml. See Cannell’s discussion of this at the end of this article- The blood level needed to cure Lupus is likely 100 to 150 ng/ml, so who knows how many more genes get turned on and off at these extra high levels? (more research please).
So- what is lupus? You may have seen people with its telltale butterfly rash on the face like the singer Seal-
Or you may have heard of the singer Selena Gomez undergoing a kidney transplant to replace one of her lupus-damaged kidneys.

(Note: Someone should tell Ms. Gomez to look into taking high dose Vitamin D3 to prevent further damage to her new kidney!)
Again, So-what is lupus?
From the Lupus Foundation of America December 6, 2017
Lupus is a chronic autoimmune disease that can damage any part of the body (skin, joints, and/or organs). “Chronic” means that the signs and symptoms tend to last longer than six weeks and often for many years.
In lupus, something goes wrong with the immune system, which is the part of the body that fights off viruses, bacteria, and germs (“foreign invaders,” like the flu). Normally our immune systems produce proteins called “antibodies” which protect the body from these invaders.
“Autoimmunity” means your immune system cannot tell the difference between these foreign invaders and your body’s healthy tissues (“auto” means “self”). As a result, it creates autoantibodies that attack and destroy healthy tissue. These autoantibodies cause inflammation, pain, and damage in various parts of the body. It can destroy kidneys, joints, skin, hair, lungs, heart, hair, and muscle.
Lupus takes its name from the Latin word “lupus”, meaning wolf. This is because a lupus-caused rash on a person’s face makes the person’s face look like the face of a wolf
The various visible manifestations of lupus:




 Now before I provide you with the testimonials of people who are CURING their Lupus with high dose Vitamin D3 with no side effects and for a cost of next to nothing (maybe $50 a year if you buy Vitamins D3 and K2 as bulk powder), let’s see what modern medicine and Big Pharma have to treat lupus?
Now before I provide you with the testimonials of people who are CURING their Lupus with high dose Vitamin D3 with no side effects and for a cost of next to nothing (maybe $50 a year if you buy Vitamins D3 and K2 as bulk powder), let’s see what modern medicine and Big Pharma have to treat lupus?
Of course the drug of choice is going to cost more than gold- how about $35,000 per year for life!??
Cost of lupus medications
A new treatment for lupus, given through IV infusion, Benlysta costs about $35,000 per year, according to the National Institutes of Health. According to a fact sheet from the Lupus Foundation of America, the yearly cost of treatment for lupus averages more than $12,600 per patient if you go with the cheaper choices.
What side effects have been found with BENLYSTA? BENLYSTA was generally well-tolerated. The most commonly reported adverse reactions with BENLYSTA were nausea, diarrhea, fever, inflammation of the nose and throat, bronchitis, insomnia, pain in extremity, depression, and migraine.
Other drugs used to treat Lupus-each with their own risk of side effects are as follows:
Aspirin-Bleeding
Acetaminophen (Tylenol®)-Liver damage (especially if you drink alcohol)
Ibuprofen (Motrin®), naproxen (Naprosyn®), indomethacin (Indocin®), nabumetone (Relafen®), and celecoxib (Celebrex®). -Bleeding
- Inflammation suppression.
- Especially useful for joint pain and stiffness.
- People often respond better to one particular NSAID than another so you may need to try several different products to determine the most effective one for you.
- Like aspirin, NSAIDs can cause stomach irritation.
- NSAIDs may also cause serious gastrointestinal (GI) complications, such as a bleeding ulcer.
Corticosteroids
(also known as glucocorticoids, cortisone or steroids) are synthetic (man-made) prescription drugs designed to work like the body’s naturally occurring hormones produced by the adrenal glands, in particular cortisol. Steroid medications work quickly to decrease the swelling, warmth, tenderness and pain that are associated with inflammation. They do this by lessening the immune system’s response. Prednisone is the most commonly prescribed steroid for lupus. Prednisolone and methylprednisolone (Medrol®) are similar to prednisone. Some physicians prefer to prescribe these if you have liver problems. Your doctor will try to keep your steroid dosage at the lowest effective level.
Steroids can produce a variety of side effects, including:
- Acne
- A round or moon-shaped face, weight gain or hair growth
- Fluid retention and a redistribution of fat, leading to a swollen face and abdomen but thin arms and legs
- Fragile skin that bruises easily.
- Suppressed growth in children.
- Irritability, agitation, excitability, insomnia or depression.
Changes in appearance and mood are more apparent with high doses of steroids.
Long-term steroid use can produce additional side effects, including:
- Increased risk of infections poses the most danger. If you are taking steroids, you must take extra care to clean and protect any open wounds. Infections are one of the leading causes of death in people with lupus.
- Avascular necrosis of bone, which occurs most often in the hip, is the destruction of the bone itself and is quite painful. Relief from pain often requires total joint replacement.
- Osteoporosis (bones become fragile and more likely to break) leads to bone fractures, especially compression fractures of the vertebrae with severe back pain.
- Muscle weakness and cataracts also can occur.
Infections are one of the leading causes of death in people with lupus. Long-term steroid use can increase your risk of infection. If you are taking steroids, take extra care to clean and protect any open wounds.
Anti-malarials
Antimalarials are prescription drugs used in combination with steroids and other medications, in part to reduce the dose required of the other drugs. Antimalarials are most often prescribed for skin rashes, mouth ulcers and joint pain, but also can be effective in mild forms of lupus where inflammation and blood clotting are a concern. Antimalarials improve lupus by decreasing autoantibody production, protecting against the damaging effects of ultraviolet light from the sun and other sources and improving skin lesions. The two types of antimalarials most often prescribed today for lupus are hydroxychloroquine (Plaquenil®) and chloroquine (Aralen®). Unlike the rapid response seen with steroids, it may take months before antimalarial drugs improve your lupus symptoms. Side effects from antimalarials are rare and usually mild; they include upset stomach and changes in skin color. In high doses and over time, certain antimalarial drugs may damage the retina of the eye (retinal toxicity), causing vision problems. Long term plaquenil users on high doses will need to monitor eye health regularly to prevent retinal toxicity from long-term use.
Immunosuppressives (Immune Modulators)
Immunosuppressive medications are prescription drugs used to control inflammation and the overactive immune system, especially when steroids have been unable to bring lupus symptoms under control, or when a person cannot tolerate high doses of steroids. However, there can be serious side effects from these drugs. Immunosuppressive drugs reduce your body’s ability to fight off infections and increase the chances that you could develop viral infections such as shingles (chicken pox or herpes zoster). These drugs may also increase your risk for developing certain types of cancer. Each immunosuppressive drug has unique side effects.
Cyclophosphamide (Cytoxan®)
- Originally developed as a chemotherapy drug (to treat cancer) and used as an immunosuppressant (to treat lupus).
- Can affect a woman’s menstrual cycle.
- Can cause bladder problems, hair loss and sterility.
Methotrexate (Rheumatrex™)
- Originally developed as a chemotherapy drug (to treat cancer) and used as an immunosuppressant (to treat lupus).
- Known as the “gold standard” — the best drug — for the treatment of rheumatoid arthritis.
- Shown to be very effective in treating skin lesions, arthritis and pleuritis in people with lupus.
- Can cause sun-sensitivity, liver damage, including cirrhosis and lung infections.
- Nausea, mouth sores and headaches are the most common side effects.
- If you are taking this drug you should not drink alcohol, especially if you have a history of kidney disease. If you are taking high-dose of methotrexate, you should not use NSAIDs; caution is also advised when taking aspirin.
Azathioprine (Imuran®)
- Developed to prevent rejection of kidney transplants.
- Blocks inflammation pathways in lupus.
- Can cause pancreatitis and an allergic form of hepatitis, so liver function tests and blood counts should be done regularly.
Anticoagulants
Because blood clots can be a life-threatening symptom of lupus, these drugs thin the blood to prevent it from clotting too easily. Anticoagulant medications include low-dose aspirin and prescription heparin (Calciparine®, Liquaemin®) and warfarin (Coumadin®). In particular, if you are being treated with warfarin, you must be monitored by your doctor to be sure your blood does not become too thin.
Monoclonal antibodies (mAbs)
Benlysta® (belimumab, formerly called LymphoStat-B™) was developed to disrupt activation of B lymphocytes by interfering with BLyS, a protein required for B cell activity. Benlysta is the first and only drug specifically developed for and approved to treat lupus.
Repository Corticotropin Injection (H.P. Acthar Gel)
Acthar® contains a naturally occurring, highly purified hormone called ACTH, which stands for adrenocorticotropic (a-DRE-no-cor-ti-co-TRO-pic) hormone. One way Acthar is thought to work is by helping your body produce its own natural steroid hormones, such as cortisol. These hormones may assist your immune system by helping your body defend itself against inflammation.
So that’s quite a list! And whatever treatment you choose you will have to remain on it the rest of your life, or until you die from an infection caused by immune system suppressants.
Now what if I told you there is a seco-steroid hormone that is not on the above list that knows which of the hundreds if not thousands of immune system genes to turn off and which ones to turn on to completely eradicate your Lupus that will cost you maybe $50 at most and will not just treat your lupus but will CURE IT!??
You would love this idea- but Big Pharma and possibly some doctors would hate it! There is no profit in a cure!
Well that miracle treatment is as close as your local grocery store with a Vitamin isle! Run and go get yourself some Vitamin D3 and you will also want to take Vitamin k2 with it to make it safe.
How much Vitamin D3 will you need to cure your Lupus? I have heard from one lady who only needed 10,000 IU per day for a few months to get very good results- you can read her testimonial shortly. Another case is of a lady who had taken 40,000 IU per day to completely knock out her Lupus-see her testimonial -shortly. These additional testimonials come from the Dr. Coimbra protocol web page.
Vitamin D3 pills at the store are often quite cheap compared to all Big Pharma drugs, but Vitamin K2 can cost more than $6,500 per gram in pill form if you buy a brand such as Dr Mercola’s. This is 30X the cost of gold! If you buy bulk powder vitamin K2 it will cost only $15 per gram! Quite a difference no?
Why do you need Vitamin K2 with high dose Vitamin D3? Because high dose Vitamin D3 remodels your immune system but also remodels your bones and joints and other tissues if they need repair of any kind. This can lead to excess calcium being deposited into your blood, But the vitamin K2 recharges a hormone (osteocalcin) that puts the calcium back in your bones where it belongs. Vitamin D3 therapy can deplete your Vitamin K2 levels which could lead to symptoms such as calcium kidney stones if not corrected. This is extremely rare however as I have heard of kidney stones forming in only about 2 out of 1,000+ high dose vitamin D3 experiments that people have reported to me. In both cases, it took about 5 months of 50,000 IU per day of D3 for the stones to form and these two people were not taking any vitamin K2. Nor were they testing their blood for calcium. Also, one of them had a brother who had developed kidney stones in his 20’s. Again this complication is very rare and not dangerous but just painful when the stone passes.
It is a simple matter to just get an occasional blood calcium test and if it is normal then there is nothing to worry about no matter how much D3 you are taking ! I know of one man who takes 1 million IU’s of D3 per day for MS 9and lots of K2) and his blood calcium continues to stay in the low normal range. See my article on the MS cure that is sweeping the planet! (I do not recommend this dose for normal people however without careful blood testing). The Dr. Coimbra protocol to cure all autoimmune diseases suggests a dose of 1,000 IU per day of Vitamin D3 per each kg of body weight.
One last note, if you are going to take high dose D3 you might also want to take a daily magnesium supplement because in rare cases the D3 can use up too much of your magnesium and you might get magnesium deficiency symptoms which can include twitching, cramps, and even panic attacks! Again, this is quite rare…but a simple risk that is easy to avoid.
Okay enough about the Lupus disease, let’s hear about the Lupus cure-from cured people in their own words!>>
Case #1- (10,000 IU per day)
(this was a review of the book- The Miraculous Results Of Extremely High Doses Of The Sunshine Hormone Vitamin D3 My Experiment With Huge Doses Of D3 From 25,000 To 50,000 To 100,000 Iu A Day Over A 1 Year Period Paperback – September 2, 2013
Great Information!!
By Amazon Customer on September 12, 2013
Format: Kindle Edition|Verified Purchase
I am very fortunate to have found this ebook. I had a Vit D test on July 25, 2013 and my test number was 18. It did not surprise me because I have been at these low numbers for years and did nothing about it. My doctors were never concerned about it and neither was I since I did not know better. I am female and 54 years old. In 1997 my body started falling apart and fifteen doctors and thousands of dollars spent trying to find a solution to my medical problems. I was referred to different doctors for different problems. I have discoid lupus on my scalp which caused quite a bit of hair loss, horrible skin breakouts and lesions on my scalp, face, chest and arms. I started loosing my eyebrows and eyelashes. Talk about severe stress. I was at stage 5 adrenal fatigue, take thyroid medication and of course medication for the lupus problems. I could not heal with the different medications I took or the healthy foods I ate. I became allergic to the sun. If I did go outside I would break out in welts on my exposed skin. I found the e book and started taking 10,000 of Vitamin D3 with the K2 the following Monday. Four weeks later I had another blood test and my Vitamin D level was at 58. I am now seven weeks taking my Vitamin D3. My eyelashes, eyebrows and hair have started growing back in. I still have a way to go growing my scalp hair back in though. All of my welts have healed!! Nothing I did before would heal my skin. My skin is now very supple, it feels as if I have tons of lotion on. I had a root canal done two weeks ago and was put on penicillin for 10 days (endodontist said I had this problem for over a year) and for 5 of those days I stopped the Vitamin D3. My entire body started hurting again. I felt so bad. I immediately started my vitamins again and I was back to my old self again the next day. I am now able to spend time out in the sun again. It feels so good. Last week I spend time weeding my garden and got bit by several mosquitos. Usually these bites are very uncomfortable and I scratch my skin until it bleeds. NOT this time. I was bit and I did not feel any discomfort whatsoever. My skin never swelled from the bites nor did they itch. For me that was amazing. I have a doctors appointment soon and I will ask for a thyroid test and d level test to see where I am at. I want to get off of my medications. I have been wanting to up my Vitamin D3 to 20-30,000 UI. I still have a way to go. I have a bone spur and some other medical issues I want healed. The vitamins I now take are Andrews Lessmans Vitamin D3-2000UI (10,000) K1/K2 (1000), Calcium(2500) Magnesium (1200) per day. Again, thanks for the valuable information provided to us. I am planning to put my husband and brother on this program. They both need it! **My present doctor is learning as much as he can from me. I am his only patient that he knows of taking this much Vitamin D and he has noticed the huge improvement.
Case Study #2-
Cristina Minami – (50,000 per day)
Lupus April 18, 2017
“In July 2012, after many health problems, I found out that I had Lupus. I had been feeling weak, I was very thin, my red blood cells and platelets were very low, and I was diagnosed with lupus nephritis. In sum, it was all bad.
I started taking the traditional medications – corticosteroids, cyclophosphamide, reuquinol, bactrim. A cocktail of drugs. I was very swollen due to the corticoids, but gradually I got better physically, and my exams got better too.
After five cyclophosphamide sessions, my doctor asked me to take azathioprine, but that drug made me very sick. I didn’t feel well with it, I had nausea, a strange taste in my mouth. I decided to stop and stay only with the corticoid and reuquinol.
I decided to do some research, and on Facebook I found a multiple sclerosis group in which the patients followed a treatment with high doses of vitamin D. They seemed to have excellent results, with regression of the disease. I read testimonials of people who were recovering their movements and sight. I joined the group and asked about lupus. There were a few people in there with the disease, and they helped me with my doubts.
I asked my rheumatologist about high doses of vitamin D and she said she was against it, so I kept on taking reuquinol and corticosteroids. Then I got a cold. The doctor explained to me that I had to take antibiotics, even for a simple cold, even if I didn’t have a fever. She said that infections activate the lupus, and I had to take the antibiotics to prevent it. I did not want to take so many drugs for the rest of my life, and this motivated me to seek treatment with vitamin D. I got the courage to call Dr. Coimbra’s clinic.
In August of 2013 I had an appointment with Dr. Sergio Menendez, an excellent doctor, very attentive. The appointment lasted about 2 hours. But I still couldn’t find the courage to take the recommended dose of 40,000 IU per day. I started taking 10,000 IU instead, and soon realized that my health was improving. I was not getting colds so easily anymore, and I was able to lower my doses of corticoids and reuquinol.
But just a couple of months later, in October of 2013, I found out that I had developed cataracts due to the use of corticoids. The rheumatologist suspended the medication, and after two months without the corticoids, my joints started to become stiff. I remembered that I had lupus!
Finally, in January of 2014 I decided to start taking the recommended dose of 40,000 IU a day of vitamin D. After a month, the pain in my joints had completely disappeared. I went to a new appointment with Dr. Menendez, and based on my tests he increased my dose to 50,000 IU.
Today, I follow all the treatment recommendations; I drink 2.5 liters of liquids a day, avoid eating foods with too much calcium, and I have a completely normal life. The stiffness on my joints have disappeared, my kidneys work perfectly, I have no disease symptoms and my exams are excellent. Sometimes I have a cold, but I can get rid of it with lemon and propolis tea, I do not need antibiotics.
I was able to discontinue all conventional medications, my only treatment now is vitamin D. Although my rheumatologist doesn’t approve of my choice, she monitors all my exams. I think I’m proving to her that vitamin D works!
Even though this treatment has not yet been accepted and disseminated by traditional doctors, I believe that many people can benefit from it.”
Case Study #3-
Lupus Testimonials (Coimbra Protocol)
by AntonioBR » Sun Feb 26, 2017 10:01 pm
–Livia Testimonial
Livia is a girl full of life and plans, practicing Classical Ballet since she had 2 years old.
Unfortunately, 10 years ago she began to present hair loss, lost an eyebrow and developed Vasculitis in her skin and mucous membranes. She was feeling a lot of pain in her abdominal area and in her joints. She developed a severe depression and required psychotherapy and antidepressants.
The disease worsened a lot with a relapse of pericarditis and dermatological lesions. So, in the hospital she received the diagnosis of Lupus and doctors were given to her high doses of hydroxychloroquine, azathioprine and cortisone.
The side effects of these medicines soon manifested: sleeplessness, stretch marks, acne, she gained 18 kg and she lost more than 70% of her vision.
When the doctors tried to reduce the doses of the medications to minimize their side effects, symptoms of the disease worsened.
She consulted two ophthalmologists and they said that the visual impairment caused by reuquinol (hydroxychloroquine) was irreversible.
Searching on the Internet, her mom found out the Protocol of Dr. Cicero and came to see us in our clinic.
We suspend immediately all conventional medicines, and we prescribed the Protocol of vitamin D and, by extension, we withdraw the toxic food (gluten).
As the patient was high sensitivity to gluten, the success of her treatment with vitamin D Protocol is closely related to the elimination of wheat, rye, barley and oats from her diet.
Livia is following the gluten-free diet rigorously.
The evolution was simply spectacular!
Just two months after the first visit she recorded this statement-100% vision recovered, lost weight 4 kg, she is sleeping well, got out of the depression and she is very happy!
So there you have it. While there will likely never be double blind placebo controlled studies of using high dose Vitamin D3 to cure Lupus, because there is no profit in it…You can rest easy if you want to try a high dose Vitamin D3 experiment for yourself. You see taking high dose Vitamin D3 is physiologically equivalent to simply doing some intense sun tanning in the summer (which would also cure your Lupus by the way). Not so scary huh?
And the few testimonials you just read are actually not the first to have tried high dose Vitamin D3 to cure their Lupus. In fact, back around the 1940’s there were all sorts of studies being published about how high dose Vitamin D (might have been the plant based Vitamin D2 which is inferior to D3) seemed effective in treating Lupus. It was just that in the 1950’s researchers found that corticosteroids had a much more immediate effect of suppressing Lupus symptoms and it was then that all research into Vitamin D3 therapy stopped and was forgotten! Little did they know that corticosteroids did not cure Lupus but only suppressed the symptoms in the short run, but they later learned that they had serious long-term negative side effects! Instead of going back to Vitamin D3 a that point, the researchers spurred on by profits, started experimenting with patentable drugs that could make them rich, and this situation continues to this day.
Rather than use a natural hormone that seems to know exactly which genes in your immue system to turn on and turn off for a cure, the researchers keep stumbling around searching for drugs that affect some of the genes positively but can lead to serious side effects ike cancer and infections because they don’t affect all the important immune system genes in the right way. It is like they are ignoring the curative treatment and spending millions and maybe billions throwing spaghetti at the wall to see if any of it sticks! As long as they can get a net benefit of symptom suppression in most people over the net cost of people dying from side effects they are happy and file for a patent and make millions!
If you doubt any of this, please do your own research on the Pub Med search engine;. Just go to the Pub Med site and search the terms Lupus and Vitamin D and just start with the oldest entries and browse through the abstracts…. It is quite shocking that this line of research was abandoned to the higher goal of profits over patients! Here is a link for the Pub Med search engine>>
https://www.ncbi.nlm.nih.gov/pubmed/
(Pub Med is a database of almost all the medical rsearch that has been published-at least since 1967, it contains abstracts which are summaries of the medical article. It is sstartign to receive much older research which often consists of just the title of the article.)
So that’s about it! You can take responsibility for your own Lupus therapy, do just a little research and maybe cure your Lupus for $50, or give the responsibility unquestioningly to your doctor and Big Pharma who stand to make $35,000+ per year in perpetuity off of your disease.
Here are some interesting pieces of information to help you on your quest for the cure-
Epidemiology and pathogenesis of systemic lupus erythematosus
Authors: Peter H Schur, MD Bevra H Hahn, MD Section Editor:David S Pisetsky, MD, PhDDeputy Editor:Monica Ramirez Curtis, MD, MPH
EPIDEMIOLOGY
The reported prevalence of systemic lupus erythematosus (SLE) in the United States is 20 to 150 cases per 100,000 [1-3]. In women, prevalence rates vary from 164 (white) to 406 (African American) per 100,000 [2]. Due to improved detection of mild disease, the incidence nearly tripled in the last 40 years of the 20th century [4]. Estimated incidence rates are 1 to 25 per 100,000 in North America, South America, Europe, and Asia [3,5-7].
Geographic and racial distribution — Both geography and race affect the prevalence of SLE and the frequency and severity of clinical and laboratory manifestations:
- The disease appears to be more common in urban than rural areas [2,8].
- In the United States, the prevalence of SLE is higher among Asians, African Americans, African Caribbeans, and Hispanic Americans compared with Caucasians [3,5,6,8]. In European countries, the prevalence of SLE is also higher among people of Asian and African descent [3]. By comparison, SLE occurs infrequently in Africa [3,9].
- In New Zealand, the prevalence and mortality of SLE are higher in Polynesians than Caucasians [10].
Incidence of Lupus over time-
Rheumatology (Oxford). 2017 Nov 1;56(11):1945-1961. doi: 10.1093/rheumatology/kex260.
The worldwide incidence and prevalence of systemic lupus erythematosus: a systematic review of epidemiological studies.
Rees F1,2, Doherty M1, Grainge MJ3, Lanyon P1,2, Zhang W1.
Abstract
OBJECTIVES:
The aim was to review the worldwide incidence and prevalence of SLE and variation with age, sex, ethnicity and time.
METHODS:
A systematic search of MEDLINE and EMBASE search engines was carried out using Medical Subject Headings and keyword search terms for Systemic Lupus Erythematosus combined with incidence, prevalence and epidemiology in August 2013 and updated in September 2016. Author, journal, year of publication, country, region, case-finding method, study period, number of incident or prevalent cases, incidence (per 100 000 person-years) or prevalence (per 100 000 persons) and age, sex or ethnic group-specific incidence or prevalence were collected.
RESULTS:
The highest estimates of incidence and prevalence of SLE were in North America [23.2/100 000 person-years (95% CI: 23.4, 24.0) and 241/100 000 people (95% CI: 130, 352), respectively]. The lowest incidences of SLE were reported in Africa and Ukraine (0.3/100 000 person-years), and the lowest prevalence was in Northern Australia (0 cases in a sample of 847 people). Women were more frequently affected than men for every age and ethnic group. Incidence peaked in middle adulthood and occurred later for men. People of Black ethnicity had the highest incidence and prevalence of SLE, whereas those with White ethnicity had the lowest incidence and prevalence. There appeared to be an increasing trend of SLE prevalence with time.
CONCLUSION:
There are worldwide differences in the incidence and prevalence of SLE that vary with sex, age, ethnicity and time. Further study of genetic and environmental risk factors may explain the reasons for these differences. More epidemiological studies in Africa are warranted.
© The Author 2017. Published by Oxford University Press on behalf of the British Society for Rheumatology. All rights reserved. For Permissions, please email: journals.permissions@oup.com
Randomized controlled trial: Vitamin D and gene expression
Posted on: April 6, 2013 by John Cannell, MD
Randomized controlled trial: Vitamin D and gene expression
We know that vitamin D controls from anywhere between 0. 5% of the human genome to up to 5%, depending on what review one reads. New genes are being discovered every day that vitamin D either upregulates or down regulates. That is, vitamin D either increases or decreases the protein that gene transcribes.
However, no one has ever done a gene microarray analysis (a way of looking at a large number of genes) of patients before and after vitamin D administration. That is, no one had ever done it until Professor Michael Holick’s lab reported such a study recently in the PLoS One journal.
Doctors Arash Hossein-Nezhad, Avrim Spira and Michael Holick conducted a small randomized controlled pilot trial of 8 patients, doing a gene microarray analysis at baseline and again after two months of either 400 or 2,000 IU per day. The 2,000 IU/day group only increased 25(OH)D by 9.8 ng/ml, while 400 IU per day increased 25(OH)D by 5.6 ng/ml, so the two groups were combined for analysis. The study was conducted in the winter.
First, they found 291 genes in white blood cells that vitamin D affected. Vitamin D affects different genes in different tissues so this is only what low dose vitamin D does in white blood cells. Of the 291 genes, 82 genes were downregulated and 209 were upregulated. They found the affected gene pathways controlled immune function, transcription regulation, cell cycle activity, epigenetic modification, DNA regulation, DNA repair, and cellular response to stress.
Forty-seven of the 291 affected genes had never been reported to be affected by vitamin D. That is, they discovered 47 new vitamin D regulated genes. Even the one person who had a relatively high baseline 25(OH)D (level not given) and who obtained a 25(OH)D of above 40 ng/ml after supplementation with 2,000 IU/day for two months had differential expression of 33 genes, suggesting there is a significant genetic difference between 25(OH)D levels of 30 ng/ml and 40 ng/ml.
The authors concluded:“These results suggest that to maximize vitamin D’s effect on gene expression may require even higher doses than 2,000 IU of vitamin D3 daily.”
Yes, we think that at least 5,000 IU/day is required to obtain natural vitamin D levels. If a genetic expression difference exists between levels of 40 and 80 ng/ml, we will only learn it by further studies, similar to this breakthrough discovery by Michael Holick’s lab.
If you would like to embark on a high dose Vitamin D3 experiment to cure your Lupus, you might as well save quite a bit of money and purchase your supplements in bulk powder form with precise measuring spoons. You can learn about how to save 90%+ on supplements by reading the following article at the following link>>>
How to Save 90%+ on Vitamins, Hormones:BUY Bulk Powder-Vit K2 Can Cost 30X More Than Gold!
Very nice article! We’re all very encouraged!
I have a friend with lupus and vit. K2 is dangerous for her to take. How would you recommend she use this vit. D treament?
Hello there
thanks for writing…Are you sure that taking Vitamin K2 is dangerous for lupus patients? her doctor might be thinking of Vitamin k1 which is completely different.
Vitamin K1 helps your blood clot and some medicines are designed to interfere with this action of K1 to prevent blood clots in the veins…Vitamin k2 however does not do this it actually
just helps direct calcium out of your blood and into your bones. Vitamin K1 comes from leafy green vegetables. Vitamin K2 comes from animal products (mK4 type) or fermenting bacteria (MK7)
If she is taking a blood thinner ..you dont have to worry about vitamin K2 ….She can also get her Vitamin k2 by eating saurkraut, or brie and gouda cheeses, or butter from grass fed cows (Spring and summer grass) or eatgn a stinky jap[anese dish of fermented soybeans called natto (the highest levels of k2 are here) sold at asian grocery stores. As long as she takes 20,000 ius of d3 per day or less she probably does not have to worry about the k2 so much….Check out the Dr. Coimbra protocol for lupus on the internet he uses very ghih doses without K2…and just has his patients avoid milk cheese and calcium rich foods…and drink extra water to avoid getting caclcium kidney stones.